Dr. Prashant Kumar
-
Everyday
10:00 AM to 5:00 PM
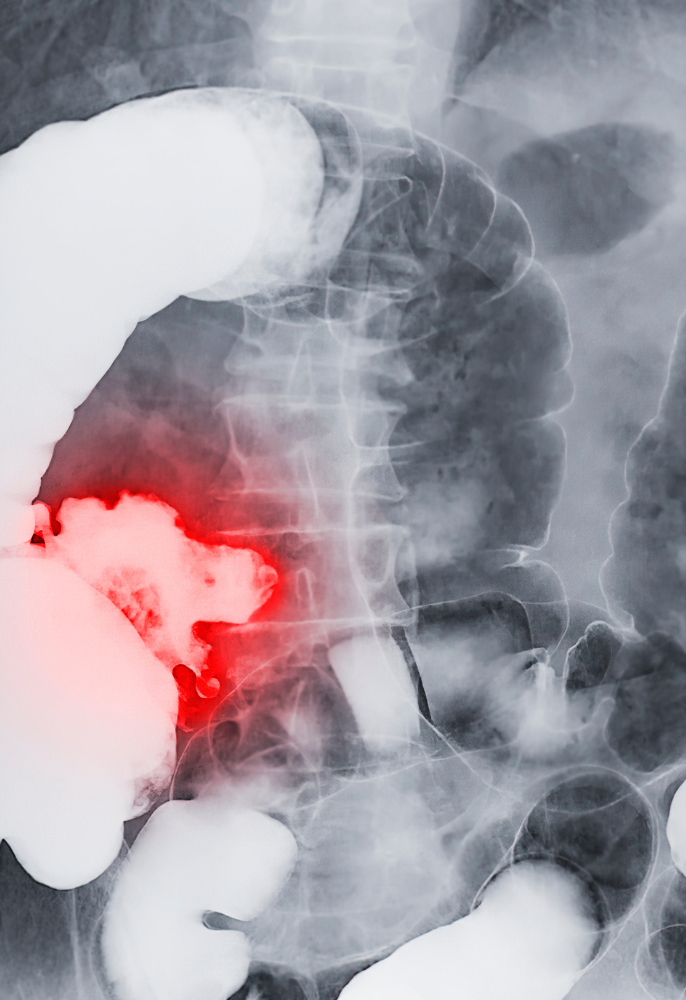
Colon and Rectal (Colorectal) Cancers are one of the most common cancers that afflict many people around the world. It is a growth that occurs in our large intestine. It is also commonly known as ‘Bowel Cancer’. The Colon is commonly known as the large intestine (bowel), and it starts after the small intestine (near where the appendix arises) and ends at the Rectum. The Colon continues into the Rectum. The Rectum is the last part of the ‘Large Intestine’ and the Rectum ends at the anus. A Cancer is a growth which is made up of abnormal cells that have ‘lost control’. Thus, cancers grow and can invade and spread to other organs. This uncontrolled growth makes cancers dangerous and life threatening
We believe that many Colorectal Cancers begin as ‘Polyps’. Colorectal Polyps are growths that occur in the Colon and Rectum. Many polyps are benign (non-cancerous). However, some polyps, if left long enough, may change in nature, and transform into cancers. This is known as the ‘Polyp-Cancer Sequence’. Some Colorectal Cancers, however, do not go through this ‘Polyp-Cancer sequence’ and start off directly as cancers
Many studies have shown benefit from screening of Colorectal Cancer. While the cost-benefit of population screening is contentious in less developed economies, the Screening of Increased (High) - Risk populations is undoubtedly worthwhile and recommended. Colonoscopy Screening is recommended for people who belong to Increased-Risk Groups. This includes people with a family history, especially first-degree relatives, of Colorectal cancer, a personal or family history of polyps.

The main treatment of Colorectal Cancer is Surgery. Adjuvant/Additional treatment with Chemotherapy and Radiotherapy has added to the improved results and prognosis in many patients.
Many Colorectal Cancers can be removed surgically. Surgery by an experienced Surgeon is associated with Low Risks, Low Morbidity and Low Local Recurrence rates. Distant metastases are reduced with chemotherapy.
Early detection of cancer
The detection of polyps – which are usually without symptoms
Removal of pre-cancerous polyps which may then reduce the chance of one developing colorectal cancer
‘Screening’ means to subject an Individual who has no symptoms or complaints for a test to look for or rule-out a disease or early signs of the disease. An individual who has symptoms and signs undergoes ‘investigation’ (not screening) of a disease.
General population screening for Colorectal Cancer is recommended in most countries where healthcare systems are well developed. While the cost-benefit of population screening is contentious in less developed economies, the Screening of Increased-Risk populations is undoubtedly worthwhile and recommended.
Colonoscopy Screening is especially recommended for people who belong to ‘Increased-Risk’
Groups. This includes individuals with a family history of Colorectal cancer (especially first-degree relatives), a personal or family history of polyps.
Treatment for Colon and Rectal Cancers usually involves surgery at some point. Although the term ‘Colorectal’ Cancer is used widely, Colon Cancers and Rectal Cancers are approached slightly differently.
The Colon starts from the Cecum and where the small intestine joins the large intestine. It ends at the Sigmoid Colon. The Rectum starts at where the Sigmoid Colon ends and ends at the top of the anal canal (which is the anus). The Recto-Sigmoid Junction is where the Colon and Rectum meet. The terminology is confusing even for many doctors who are not well versed with treatment for Colorectal Cancer.
The reason of this differentiation is that Colon Cancers tend to spread or recur differently from Rectal Cancers. Rectal Cancer treatment can also be much more challenging due to the location in the confines of the pelvis which can be very limited in space, especially in males and obesity.
Local recurrence (recurrence at or around the site of surgery or anastomosis) of Colon Cancers is uncommon and the recurrences and spread tend to be to other organs and areas.
Rectal Cancers recur locally (i.e. at or around the site of surgery in the pelvis or anastomosis – where the joint takes place) more frequently than Colon Cancers. Good surgical techniques are important and are targeted at good and meticulous clearance of the surrounding tissue.
Although overall, local recurrences rates are low, surgery performed by good and experienced Colorectal surgeons are noted to have lower local recurrence rates for Rectal Cancers.
Additional Treatment for Rectal Cancers like Radiotherapy and Chemotherapy also have reduced local recurrence rates.
Distant recurrence of Colon and Rectal Cancers are reduced with adjuvant Chemotherapy, and the newer forms of targeted Immunotherapy.
Surgery entails removing the following en-bloc (in 1 piece together): The Cancer itself
Together with an adequate margin of normal colon/rectum without cancer cells
The surrounding mesentery where the lymph nodes and blood vessels supplying that segment are situated
Division of the origin of the blood vessels supplying the segment
The surrounding fat (mesorectum) attached to the rectum in rectal cancers
Conventional Surgery
Conventional Surgery is performed with usually large incisions. This results in more post-operative pain and longer recovery. Many Colorectal Surgical Procedures are now
performed Laparoscopically (Key-Hole Surgery). However, sometimes, for various reasons like large cancers, infiltration to surrounding areas, previous surgery causing adhesions etc, conventional surgery may still have to be performed.
LaparoscopicSurgery Robotic Surgery
Robotic Surgery is a recent modality for performing surgery. Robotic Surgery has been proven superior in Prostate Cancer Surgery. However, its use in many other surgical procedures is still controversial.
In my opinion, Robotic Surgery may have advantages in performing some difficult Rectal Cancer Surgery. However, it may not be essential.
Colostomy / Bag to pass motion into
Perhaps the single factor that concerns many patients when told that they have Colorectal Cancer is the thought of having a permanent Colostomy. A Colostomy is when the colon/intestine is brought out to a hole in the abdominal wall and stools are passed into a bag that is attached to the skin instead of passing stools through the anus.
Many patients, who are unaware, are afraid of having a colostomy. Some patients, who have not been adequately counselled, even go to the extent of declining Cancer Treatment and Surgery because of the possibility that a permanent Colostomy is required.
Permanent Colostomies used to be common. However, with experienced Colorectal surgeons, new technology and surgical equipment, the number of patients who require permanent colostomies have reduced.
The use of a Temporary Colostomy/Ileostomy is fairly common in surgery for mid to low Rectal Cancers and is part of a staged process in surgery. Usually, after the anastomosis (joint of the rectum) has healed, a smaller surgical procedure is performed to close/remove the colostomy/Ileostomy so that the patient can move bowels through the anus again.
Patients are encouraged to discuss openly with their surgeons about colostomies and not be afraid. Although, in present day, many permanent colostomies can be avoided, some patients will still require permanent colostomies to ensure adequate clearance of the cancer. It would be foolish to decline treatment of the cancer purely because a colostomy is required. Patients who
do, eventually suffer as the untreated cancer grows or is not treated adequately, and ultimately, do still require a colostomy for complications, but having lost the chance to cure the cancer.
Many patients with colostomies lead almost normal lives. There are strong support groups and allied health professionals who are on hand to assist and support patients faced with a colostomy.

Typically replies within a day
Dr Prashant Kumar Hey, Do you want to talk with us?
We Are Committed to Provide Personalised, Comprehensive & Holistic Care for You.
Mon – Sat : 10:00 AM to 5:00 PM
Sun : Closed